 In a new approach to reducing the scourge of hospital-acquired infections, a team of scientists has been testing thousands of microbe samples from a Chicago hospital to learn how a medical building might make patients sicker.
In a new approach to reducing the scourge of hospital-acquired infections, a team of scientists has been testing thousands of microbe samples from a Chicago hospital to learn how a medical building might make patients sicker.
Data from the three-year Hospital Microbiome Project are still being analyzed. So far the team has found factors including ventilation and humidity, and design features such as furnishings and fixtures, affect the kinds of bacteria people encounter inside a hospital in ways that impact their health. The scientists aim one day toslow the rise of antibiotic-resistant bacteria in hospital settings by manipulating conditions from room to room to keep pathogens in check.
They also hope eventually to make the hospital building itself a curative probiotic—perhaps by infusing walls or furnishings with bacteria that enhance patient health and recovery.
“I see a future far off where we use bacteria to protect us from the bacteria that harm us,” said infection-control epidemiologist Emily Landon at the University of Chicago’s new Center for Care and Discovery, the facility under study. “We could make the hospital itself into a treatment for the patient.”
Hospitals have done much to reduce infections contracted after patients are admitted, according to an annual survey of 14,500 U.S. hospitals by the Centers for Disease Control and Prevention. They have tightened sterilization standards, made more careful use of antimicrobials and enforced more attentive hygiene.
Still, on any given day, about 1 in 25 patients is fighting an infection contracted during hospital care, at an estimated cost of more than $36 billion a year. Hospital-acquired infections kill 75,000 people in the U.S. each year.
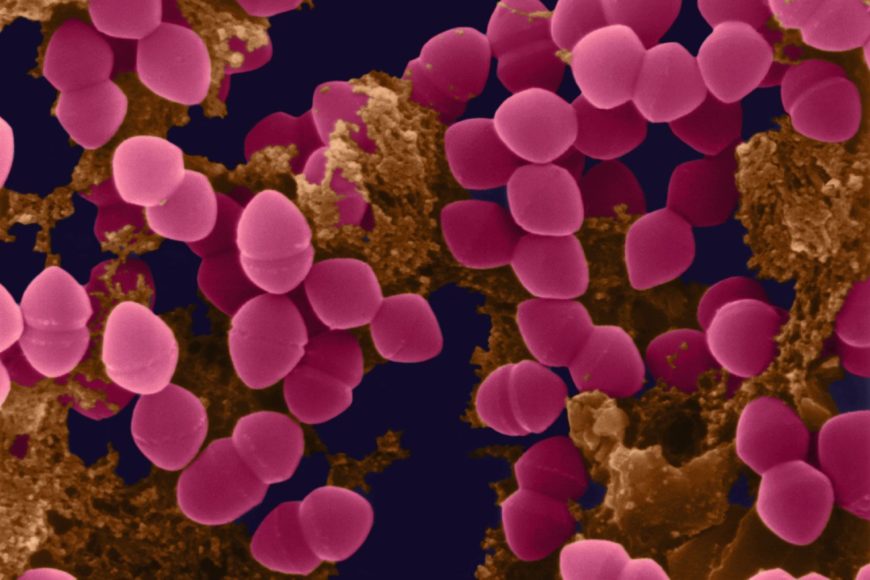
More than half of hospital infections are caused by bacteria that make themselves at home in hospital settings. Some infectious microbes cling to catheters despite rigorous hygiene efforts. Others contaminate improperly sterilized surgical areas. More than a third of hospital infections are caused by nurses and doctors who don’t wash their hands properly after a patient examination.
“Some of the hospital pathogens live both in the humans and in very expensive pieces of medical equipment that are hard to clean,” said Dr. Julie Segre, a senior scientist at the National Human Genome Research Institute in Bethesda, Md., who uses genetic analysis to track bacteria responsible for hospital infections. “That is why we worry.”
The $856,000 hospital-research project, funded by the Alfred P. Sloan Foundation in New York, stems from growing awareness that we each harbor a unique collection of a hundred trillion or so microbes in and around our bodies. This community of bacteria, called the microbiome, influences our health, mood, eating habits and sleep patterns in ways scientists are only beginning to understand.
A person typically sheds some 37 million bacteria every hour into the surrounding air or onto surfaces touched. “We leave our microbes all over the place,” said researcher James Meadow at the University of Oregon’s Biology and the Built Environment Center, who last year analyzed the microbes inhabiting a 155-room building in Eugene.
Every building appears to have its own unique microbiome, depending on how it is built and operated, who uses it and what they do there, said University of Oregon microbiologist Jessica Green, who helped pioneer the field. “We know microbes in buildings are relevant to human health,” she said.
In hospitals, for example, the air that many patients breathe, recycled through heating and air-conditioning systems, concentrates human-related bacteria and potential pathogens, compared with patient rooms with open windows where outdoor air can circulate, according to Dr. Green’s 2012 study of Providence Milwaukie Hospital in Portland.
Other recent studies discovered that moisture-loving bacteria living in showerheads include distinct populations of potential pathogens quite different from microbes on shower curtains a few feet away. Drug-resistant staph germs can live for up to a week on some common furniture fabrics. Strep germs can survive for months on a dry surface.
Experts say the Chicago hospital project is the most comprehensive effort so far to study the hidden life of a large medical facility.
About half of U.S. hospital patients take an antimicrobial drug during their stay. Half of them take two or more. The drugs kill all but the hardiest microbes, leading to generations of bacteria better able to withstand efforts to eradicate them. As broad-spectrum antibiotics decimate normal bacteria in a patient’s body, it is open for pathogens already in the room, medical experts said.
“Patients get multidrug-resistant bacteria when their bacteria are wiped out,” said Dr. Landon. Once the hospital-microbiome data are analyzed, “maybe we will find out that when a person is on antibiotics, their room needs a probiotic so that their room does not get colonized by antibiotic-resistant bacteria.”
The two dozen microbiologists and infection-control experts working on the Chicago project started collecting DNA data while the building was under construction, cataloging bacteria likely brought there by dirt, wind, water, construction materials or workers.
When the hospital officially opened on Feb. 23, 2013, the researchers documented a change in the building’s microscopic life.
“Overnight, the building became alive with all these human bacteria,” said environmental microbiologist Jack Gilbert at the U.S. Department of Energy’s Argonne National Laboratory in Lemont, Ill., who is directing the project. “The microbiome suddenly increased in diversity. It increased in complexity. There was greater variation between the spaces in the building.”
In the following year, researchers focused on a suite of five patient rooms on the hospital’s ninth floor and five rooms on the 10th floor. They installed sensors to collect information about a dozen different environmental measures that affect how bacteria grow. Every day, they collected DNA samples from beds, bed rails, water, air, room phones and other surfaces, as well as from patients, nurses and other staff.
Typically, people came in and out of each room 100 times a day, trailing invisible plumes of bacteria, the researchers found. Some room surfaces had thousands of types of bacteria; others had only a few hundred.
Within hours of arrival of a new patient, however, his or her personal collection of microbes spread throughout the room, mingling with microbes already present and making the microbiome of each room unique, Dr. Gilbert said.
Researchers hope the project will inspire a new generation of infection-control practices. Dr. Green, of the University of Oregon, believes the technology will begin showing up in hospitals within five years.
By Robert Lee Hotz Source: The Wall Street Journal
Ainda não recebemos comentários. Seja o primeiro a deixar sua opinião.





Deixe um comentário